Multiple sclerosis (MS) is more prevalent in women of childbearing age than in any other group. As a result, a key concern of many newly diagnosed women is how the disease will affect their chances of having children.

MS Patient Anna Field, 29, will begin trying for a baby in the New Year
This was the case for Anna Field, who was diagnosed with MS at the age of 26. Since her diagnosis, Anna has been on a weekly treatment of injections, which keep in check symptoms such as numbness in the body, a burning feeling in her shoulder, and Optic Neuritis (painful inflammation of the optic nerve that also causes blurred vision).
“I used to think that people with MS couldn’t have kids,” says Anna, now 29. “But when my husband and I decided we wanted to try, both my nurse and neurologist were really supportive. Information I found on the MS Trust website complemented what the specialists were saying, which was really reassuring.”
Pregnancy and MS
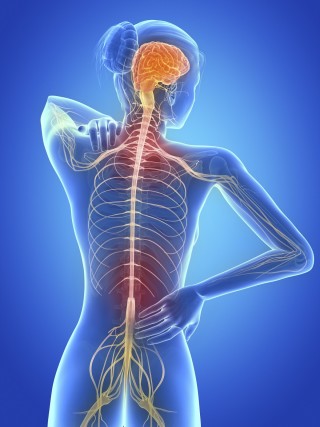
MS is a chronic, progressive neurodegenerative disorder resulting from an attack on the central nervous system (the brain, spinal cord and optical nerves) by the body’s own immune system. Symptoms vary in their form and severity but the condition can lead to worsening motor function, irreversible neurological damage and, sometimes, paralysis.
However, there’s no evidence that MS impairs fertility or increases the chance of miscarriage, stillbirth or congenital malformation. In fact, a growing body of research suggests the opposite: pregnancy seems to lessen the symptoms of MS. Women with relapsing MS frequently go into remission during their last trimester.
Decisions around medication
Doctors advise coming off medication three months before getting pregnant, so Anna has stopped her injections to begin trying for a baby in the New Year. Coming off her treatment carries risks, however, and Anna has concerns.
“I’ve been told than when you do get pregnant, symptoms often diminish and you feel better,” Anna says. “But what if I don’t get pregnant straight away? It sometimes takes people months. My other concern is that pregnancy can affect the immune system, so that after you give birth you can have a relapse.”
While Anna’s fears are not unfounded, Megan Roberts, MS specialist nurse and advanced practice advisor at the MS Trust says that, with careful planning, a healthy pregnancy is possible.
“The ideal approach is to plan ahead and ensure the woman is as stable as possible so that she can stop taking her Disease Modifying Treatment (DMT) in advance of trying for a baby,” Megan says. The MS nurse or neurologist will monitor the woman carefully and, if she develops severe symptoms, they will discuss possible options with her. While none of the DMTs can be recommended during pregnancy, some have a lower risk than others and the neurologist may discuss the option of switching to a lower risk DMT as an interim measure.
“The potential risks of the medication on the baby have to be balanced against the risks on the mother for not taking the medication,” adds Megan. “These risks will be different for everyone depending on the medication they are taking, the pattern of their MS, and their medical history.”
“There is no substitute for individual advice from a health professional. Women with MS who are hoping to get pregnant or who find that they are pregnant should always contact their MS nurse or neurologist for specific advice about any medications they are taking,” says Megan. “Once the baby has been born, the woman can restart whichever DMT is most appropriate for her, providing she’s not breastfeeding.”
Hope for MS patients: Harnessing the positive effects of pregnancy
The beneficial effect of pregnancy on MS has been attributed to hormones, as remission seems to take place when estrogen levels peak. The mechanism by which this works is not clear, but the most accepted theory is that, during pregnancy, estrogen and other sex hormones promote immunological changes that lead to an anti-inflammatory state.
A new study at the University of California, Riverside (UCR) is exploring a drug called indazole chloride (Ind-Cl) for its ability to switch on estrogen receptors in the oligodendrocytes of mice infected with MS.
So far, the drug has dramatic effects. Oligodendrocytes are cells that create myelin, the protective layer that surrounds neurons in the brain. MS destroys myelin but, in mice, Ind-Cl triggered the repair and reversal of myelin damage.
“I’m optimistic that Ind-Cl or an Ind-Cl-like drug (we have derivatives of Ind-Cl that we are testing for pre-clinical assessment) will have a significant effect on MS symptoms,” Seema Tiwari-Woodruff, associate professor in the Division of Biomedical Sciences, University of California Riverside (UCR) told the Pregnancy & Medicine Initiative. “It seems to be a very active myelin recovery drug.”
Post-pregnancy patterns
 The UCR study is further confirmation that estrogen is linked to the remission of MS symptoms. But what happens after pregnancy? Studies have shown that relapse rate often increases considerably in the first few months after the baby’s birth. Encouragingly however, long-term outlook doesn’t seem to be affected.
The UCR study is further confirmation that estrogen is linked to the remission of MS symptoms. But what happens after pregnancy? Studies have shown that relapse rate often increases considerably in the first few months after the baby’s birth. Encouragingly however, long-term outlook doesn’t seem to be affected.
A recent meta-analysis by researchers at Sapienza University and University of Ferrara, Italy, published in the European Journal of Neurology, suggested that women with MS should expect “no perceptible effect on long-term disease course or disability progression” after pregnancy. The study authors looked at retrospective data following women for up to 10 years after pregnancy.
The MS Trust has launched a new website to help people with MS understand the drug treatments available based on their personal needs. Visit it at http://www.msdecisions.org.uk/.
